- Time-based (constant attendance) CPT codes: These codes allow for variable billing in 15-minute increments when a practitioner provides a patient with one-on-one services such as therapeutic exercise or manual therapy.
- Service-based (supervised or untimed) CPT codes: These are the codes therapists use to perform services such as conducting an evaluation or applying hot/cold packs. It doesn’t matter if you complete these types of treatments in 5 minutes or 45, because you can only bill one code.
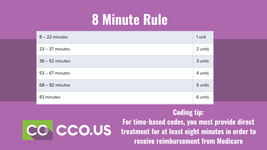
8-Minute Rule
For time-based codes, you must provide direct treatment for at least eight minutes in order to receive reimbursement from Medicare. Basically, when calculating the number of billable units for a particular date of service, Medicare adds up the total minutes of skilled, one-on-one therapy and divides that total by 15. If eight or more minutes are left over, you can bill for one more unit; if seven or fewer minutes remain, you cannot bill an additional unit.Many times, when you divide the total timed minutes by 15, you get a remainder that includes minutes from more than one service. For example, you might have 5 leftover minutes of therapeutic exercise and 3 leftover minutes of manual therapy. Individually, neither of these remainders meets the 8-minute threshold. When combined, though, they amount to 8 minutes—and per Medicare billing guidelines, that means you can bill one unit of the service with the greatest time total
The Rule of Eights—which can be found in the CPT code manual and is sometimes referred to as the AMA 8-Minute Rule—is a slight variant of CMS’s 8-Minute Rule. The Rule of Eights still counts billable units in 15-minute increments, but instead of combining the time from multiple units, the rule is applied separately to each unique timed service. Therefore, the math is also applied separately. (Keep in mind that the Rule of Eights only applies to timed codes that have 15 minutes listed as the “usual time” in the operational definition of the code.)
CPT codes actually do make allowances for assessment and management time. That time includes “all the things you have to do to deliver an intervention,” such as:
- assessing the patient prior to performing a hands-on intervention;
- assessing the patient’s response to the intervention;
- instructing, counseling, and advice-giving about at-home self-care;
- answering patient and/or caregiver questions; and
- documenting in the presence of the patient.
What is the Medicare 8-Minute Rule?
Medicare’s 8-minute rule is a stipulation that applies to time-based CPT codes for outpatient services, such as physical therapy. Introduced in December 1999, the 8-minute rule became effective on April 1, 2000.The rule allows practitioners to bill Medicare for one unit of service if its length is at least eight (but fewer than 22) minutes. A billable “unit” of service refers to the time interval for the service. Under the 8-minute rule, units of service consist of 15 minutes each.


Medicare and the 8-Minute Rule
Understanding Medicare's 8-minute rule helps make sense of how Medicare gets charged for services you receive.
www.medicarefaq.com


