What equipment, supplies, and medications are
recommended or required for a planned home
birth?
Nondisposable equipment:
Adult mask and oral airway
Fetoscope and/or Doppler device (with extra
batteries if only Doppler)
Oxygen tank with tubing and flow meter
Neonatal resuscitation mask and bag
Portable light source
Portable oral suction device for infant
Sterile birth instruments
Sterile instruments for episiotomy and repair
Stethoscope and sphygmomanometer
Tape measure
Thermometer
Timepiece with second hand
O2 saturation monitor
Medications available:
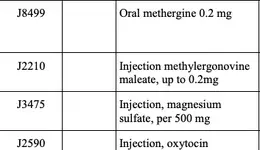
Pitocin, 10 U/ml
Methergine, 0.2 mg/ml
Epinephrine, 1:1000
MgSO4, 50% solution, minimum 2-each of
5gms in 10 cc vials
Local anesthetic for perineal repair
Vitamin K, neonatal dosage (1 mg/0.5 ml)
IV fluids, one or more liters of LR
Recommended home-birth-kit
supplies:
IV set-up supplies
Venipuncture supplies
Urinalysis supplies - clean catch cups and
dipsticks
Injection supplies suitable for maternal
needs
Injection supplies suitable for neonatal
needs
Clean gloves
Sterile gloves: pairs and/or singles in
appropriate size
Sterile urinary catheters
Sterile infant bulb syringe
Sterile cord clamps, binding equipment or
umbilical tape
Antimicrobial solution(s) for cleaning exam
room and client bathroom
Antimicrobial solution(s)/brush for hand
cleaning
Sterile amniohooks or similar devices
Cord blood collection supplies
Appropriate device for measuring newborn’s
blood sugar values
Suture supplies
Sharps disposal container, and means of
storage and disposal of sharps
Means of disposal of placenta
Required home-birth-kit supplies:
Neonatal ophthalmic ointment (or other
approved eye prophylaxis)
Risk screening criteria
The following conditions are high-risk factors. The agency does not approve or cover planned
home births or births in birthing centers for women with a history of or identified with any of
these factors.
Previous cesarean section
Current alcohol and/or drug addiction or abuse
Significant hematological disorders/coagulopathies
History of deep venous thrombosis or pulmonary embolism
Cardiovascular disease causing functional impairment
Chronic hypertension
Significant endocrine disorders including pre-existing diabetes (type I or type II)
Hepatic disorders including uncontrolled intrahepatic cholestasis of pregnancy and/or
abnormal liver function tests
Isoimmunization, including evidence of Rh sensitization/platelet sensitization
Neurologic disorders or active seizure disorders
Pulmonary disease
Renal disease
Collagen-vascular diseases
Current severe psychiatric illness
Cancer affecting site of delivery
Known multiple gestation
Known breech presentation in labor with delivery not imminent
Other significant deviations from normal as assessed by the provider
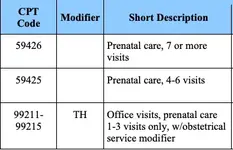
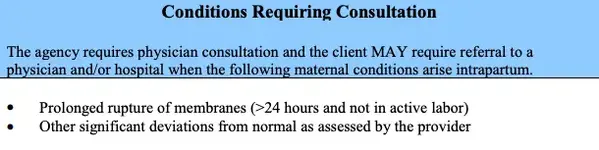
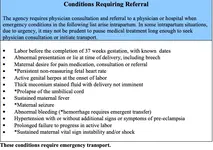
Prenatal Management/Consultation & Referral

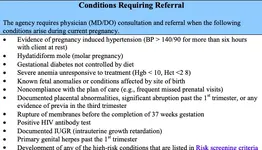
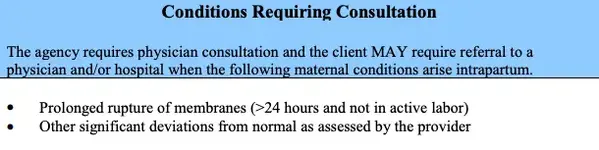
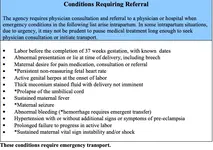
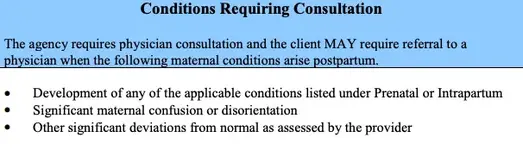
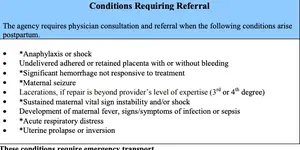
Intrapartum
recommended or required for a planned home
birth?
Nondisposable equipment:
Adult mask and oral airway
Fetoscope and/or Doppler device (with extra
batteries if only Doppler)
Oxygen tank with tubing and flow meter
Neonatal resuscitation mask and bag
Portable light source
Portable oral suction device for infant
Sterile birth instruments
Sterile instruments for episiotomy and repair
Stethoscope and sphygmomanometer
Tape measure
Thermometer
Timepiece with second hand
O2 saturation monitor
Medications available:
Pitocin, 10 U/ml
Methergine, 0.2 mg/ml
Epinephrine, 1:1000
MgSO4, 50% solution, minimum 2-each of
5gms in 10 cc vials
Local anesthetic for perineal repair
Vitamin K, neonatal dosage (1 mg/0.5 ml)
IV fluids, one or more liters of LR
Recommended home-birth-kit
supplies:
IV set-up supplies
Venipuncture supplies
Urinalysis supplies - clean catch cups and
dipsticks
Injection supplies suitable for maternal
needs
Injection supplies suitable for neonatal
needs
Clean gloves
Sterile gloves: pairs and/or singles in
appropriate size
Sterile urinary catheters
Sterile infant bulb syringe
Sterile cord clamps, binding equipment or
umbilical tape
Antimicrobial solution(s) for cleaning exam
room and client bathroom
Antimicrobial solution(s)/brush for hand
cleaning
Sterile amniohooks or similar devices
Cord blood collection supplies
Appropriate device for measuring newborn’s
blood sugar values
Suture supplies
Sharps disposal container, and means of
storage and disposal of sharps
Means of disposal of placenta
Required home-birth-kit supplies:
Neonatal ophthalmic ointment (or other
approved eye prophylaxis)
Risk screening criteria
The following conditions are high-risk factors. The agency does not approve or cover planned
home births or births in birthing centers for women with a history of or identified with any of
these factors.
Previous cesarean section
Current alcohol and/or drug addiction or abuse
Significant hematological disorders/coagulopathies
History of deep venous thrombosis or pulmonary embolism
Cardiovascular disease causing functional impairment
Chronic hypertension
Significant endocrine disorders including pre-existing diabetes (type I or type II)
Hepatic disorders including uncontrolled intrahepatic cholestasis of pregnancy and/or
abnormal liver function tests
Isoimmunization, including evidence of Rh sensitization/platelet sensitization
Neurologic disorders or active seizure disorders
Pulmonary disease
Renal disease
Collagen-vascular diseases
Current severe psychiatric illness
Cancer affecting site of delivery
Known multiple gestation
Known breech presentation in labor with delivery not imminent
Other significant deviations from normal as assessed by the provider
Prenatal Management/Consultation & Referral

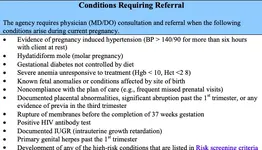
Intrapartum