Coding for Home Heath can be tricky. There are rules to follow. Selecting a Primary DX is key.
Coding under PDGM
1. Align OASIS ICDs with Referral Documentation from the Physician
Medicare regulations require that a physician, with a current and active physician license, must order home health care services. The HHA must obtain written documentation of the physician’s home health care order. The order can be documented by the physician in several ways: Discharge Summary, Referral, Patient Assessment, History and Physical, Physician Progress report. The written summary may or may not actually contain the diagnoses codes you will use on the OASIS assessment. If the document does not have the actual ICD-10-CM code, you must select the most appropriate code from the ICD-10-CM list. If the report has the actual diagnosis codes, you’ll use those codes.How to Select the Primary Diagnosis
The primary reason for home care, i.e. OASIS item M1021, is always the primary diagnosis. The physician who signs the plan of care (CMS485), i.e. the ‘certifying’ physician (as opposed to the ‘referring’ physician’) always determines the primary diagnosis and documents this during the face-to-face encounter required by Medicare.
The primary diagnosis must have a Patient-Driven Groupings Model (PDGM) classification.
The primary diagnosis must have one of twelve PDGM classifications according to home health care coding guidelines. Of the more than 70,000 ICD-10-CM diagnosis Codes, about 43,000 have PDGM classifications and can be used as a primary diagnosis. Click here to access the list of ICD-10-CM Diagnosis codes that have a PDGM classification.
Home Health Coding: Medicare Do's & Don'ts under PDGM
Make sure your home health coding follows Medicare Conditions of Participation (CoPs).
Medicare provides this resource. It includes fee for service info.
Coding and Billing Information | CMS
Home Health PPS Coding and Billing Information includes:
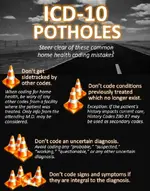
The following are some of the guidelines that CMS spelled out in the November 2018 Federal Register that must be followed for coding under PDGM.
- Whenever possible, the most specific code that describes a medical disease, condition, or injury should be documented.
- Generally, ‘‘unspecified’’ codes are used when there is lack of information about location or severity of medical conditions in the medical record.
- Provider is to use a precise code whenever more specific codes are available.
- If additional information regarding the diagnosis is needed, the HHA is to follow-up with the referring provider in order to ensure the care plan is sufficient in meeting the needs of the patient.
- Vague principal diagnosis does not clearly identify the primary reason for home health, and subsequently leads to ambiguous resource use.
- A home health clinician should not report an ‘‘unspecified’’ code if that clinician can identify the laterality or site of a condition.
- Many symptom codes, such as pain or contractures cannot be used as the primary diagnosis: For example, 5, Low back pain or M62.422, Contracture of muscle, right hand, although site specific, do not indicate the cause of the pain or contracture. In order to appropriately group the home health period, an agency will need a more definitive diagnosis indicating the cause of the pain or contracture, as the reason for the skilled care.
- R Codes (which are symptoms, signs, and abnormal clinical and laboratory findings, not elsewhere classified) are not allowed as a primary diagnosis, except for a few dysphagia codes. In the CY 2020 Final Rule, CMS determined that given the current lack of other definitive diagnoses to describe certain forms of dysphagia, the R-codes to describe dysphagia would be acceptable for reporting the primary reason for home health services. Therefore, the following R-codes will be assigned to the Neuro Rehab clinical group:
- R13.10, R13.11, R13.12, R13.13, R13.14 & R13.19 – Multiple Dysphagia codes
- CMS recognizes that the coding guidelines allow for the reporting of signs, symptoms, and less well-defined conditions, however, HHAs are required to establish an individualized plan of care in accordance with the home health CoPs at § 484.60.
- CMS believes that the use of symptoms, signs, and abnormal clinical and laboratory findings would make it difficult to meet the requirements of an individualized plan of care.
- Clinically it is important for home health clinicians to have a clearer understanding of the patients’ diagnoses in order to safely and effectively furnish home health services.
- For patient safety and quality of care, it is important for a clinician to investigate the cause of the signs and/or symptoms for which the referral was made.
- This may involve calling the referring physician to gather more information in order to establish the underlying cause.
- Muscle weakness is another unacceptable code as a Primary Diagnosis under PDGM. CMS has stated that:
- M62.81, ‘‘Muscle weakness, generalized’’ is extremely vague.
- Generalized muscle weakness, while obviously a common condition among recently hospitalized patients does not clearly support a rationale for skilled services and does not lend itself to a comprehensive plan of care.
- If there is not an identified cause of muscle weakness, then it would be questionable as to whether the course of therapy treatment would be in accordance with accepted professional standards of clinical practice.
- CMS identified ‘‘muscle weakness (generalized)’’ as a nonspecific condition that represents general symptomatic complaints in the elderly population.
- S and T codes
- There are many of the S and T codes where the fracture and/or injury is unspecified, but the site is specified.
- CMS maintains that the site of injury and/or fracture should be identified; however, the treatment or intervention would likely not change based on the exact type of injury or fracture.
- Many of these codes are appropriate to group into a clinical group, and are assigned to either the musculoskeletal group or the wounds group.
- Based on the primary diagnosis, each 30-day period is placed into one of the 12 clinical groupings – HHAs should be familiar with codes that are used to group 30- day periods of care into the 12 clinical groupings.
- If the primary diagnosis does not fit into one of the 12 clinical groups in the payment model, this is considered a “Unacceptable Diagnosis”.
- There are 14 subgroups that can receive a low comorbidity adjustment
- There are 31 High Comorbidity Adjustment Interaction Subgroups, however, 20 of the subgroups have interactions with either a non-pressure chronic ulcer or with a pressure ulcer

Diagnosis Coding for Home Care – Tips for Success
As the first year of PDGM has unfolded there have been many twists and turns in the new complexity of coding in home care. Many of the diagnosis codes we had been utilizing in home health, are no longer allowed as a primary diagnosis, called unacceptable primary diagnoses. Coding has always been...
 healthcareprovidersolutions.com
healthcareprovidersolutions.com
How to Bill Medicare for all Home Health Eligible Claims.
Medicare provides for 3 methods of reimbursement for Physicians who
refer patients to a Medicare Certified Home Health Agency:
1. Physician Certification (Billing Code G0180)
Physician Certification of Home Health Plan of Care is defined as physician
services for initial certification of Medicare-covered home health services
2. Physician Re-Certification (Billing Code G0179)
Physician re-certification is used when the physician signs the Plan of Care
(Form 485) to re-certify a patient for home health services. A physician will
re-certify a patient after a 60 day certification period.
3. Physician Care Plan Oversight (CPO) (Billing Code G0181)
Physicians can bill for 30 minutes of Care Plan Oversight that includes
supervision of a complicated patient and requires extensive review /revision
of care plans, review of laboratory or study results, phone calls to other
health professionals, and other activities associated with the patient’s home
health care.

Diagnosis Coding for Home Care – Tips for Success
As the first year of PDGM has unfolded there have been many twists and turns in the new complexity of coding in home care. Many of the diagnosis codes we had been utilizing in home health, are no longer allowed as a primary diagnosis, called unacceptable primary diagnoses. Coding has always been...
 healthcareprovidersolutions.com
healthcareprovidersolutions.com
Last edited: