Medicare’s Annual Wellness Visit (AWV)
The Medicare Annual Wellness Visit (AWV) is a yearly appointment with a health professional to identify health risks and help reduce them and to create or update a personalized prevention plan. During a Medicare AWV, health professionals should also review any current opioid prescriptions, detect any cognitive impairment, and establish or update medical and family history.
Coding and Billing a Medicare AWV
G0438: Annual wellness visit, includes a personalized prevention plan of service (PPS), initial visit
G0439: Annual wellness visit, includes a personalized prevention plan of service (PPS), subsequent visit
G0468: Federally qualified health center (FQHC) visit, IPPE, or AWV; a FQHC visit that includes an initial preventive physical examination (IPPE) or annual wellness visit (AWV) and includes a typical bundle of Medicare-covered services that would be furnished per diem to a patient receiving IPPE or AWV
Diagnosis code Z00.00; Initial Annual Wellness Visit G0438; Subsequent Annual Wellness Visit G0439
Medicare will pay a physician for an AWV service and a medically necessary service, e.g. a mid-level established office visit, Current Procedural Terminology (CPT) code 99213, furnished during a single beneficiary encounter. It is important that the elements of the AWV not be replicated in the medically necessary service. Physicians must append modifier -25 (significant, separately identifiable service) to the medically necessary E/M service, e.g. 99213-25, to be paid for both services.
For example, for the patient who comes in for his Annual Wellness Visit and complains of knee tendonitis would be billed as follows: CPT ICD-10, G0438 Z00.00, 99212-25 M76.50 (tendonitis)
Medicare annual wellness exams
Preventive services for fee-for-service Medicare beneficiaries has been expanded in addition to the once-ever Welcome to Medicare visit availability in the first 12 months of Medicare enrollment, beneficiaries can receive an
annual wellness and prevention exam with no copay (i.e. free) to the beneficiary.
Billing is not done using the normal wellness-exam CPT codes (
99381-99397) – such claims will be rejected by Medicare as “non-covered services” – but instead one uses new, Medicare-only codes: G0438 for initial visits, and G0439 for subsequent visits.
Annual Wellness Visit
Diagnosis code Z00.00; Initial Annual Wellness Visit G0438; Subsequent Annual Wellness Visit G0439
Medicare will pay a physician for an AWV service and a medically necessary service, e.g. a mid-level established office visit, Current Procedural Terminology (CPT) code 99213, furnished during a single beneficiary encounter. It is important that the elements of the AWV not be replicated in the medically necessary service. Physicians must append modifier -25 (significant, separately identifiable service) to the medically necessary E/M service, e.g. 99213-25, to be paid for both services.
The
Annual Wellness Visits video helps health care professionals understand these exams and their purpose, and the requirements when submitting claims for them.
Medicare Physical Exams Coverage
Initial Preventive Physical Exam (IPPE)
Review of medical and social health history and preventive services education.
✔ New Medicare patients within 12 months of first Part B coverage period
✔ Patients pay nothing (if provider accepts assignment)
Annual Wellness Visit (AWV)
Visit to develop or update a Personalized Prevention Plan (PPP) and perform a Health Risk Assessment (HRA).
✔ Covered once every 12 months
✔ Patients pay nothing (if provider accepts assignment)
Routine Physical Exam
Exam performed without relationship to treatment or diagnosis for a specific illness, symptom, complaint, or injury.
✘ Medicare doesn’t cover a routine physical (it’s prohibited by
statute), but the IPPE, AWV, or other Medicare benefits cover certain routine physical elements
✘ Patients pay 100% out-of-pocket
Please see the denials thread here for more info on denials:
Review Reason Codes and Statements CMS contractors medically review some claims (and prior authorizations) to ensure that payment is billed (or authorization requested) only for services that meet all Medicare rules. If the review results in a denied/non-affirmed decision, the review contractor...

www.cco.community
Common reasons for denial include the folllowing:
1. Billing a G0438 (initial Medicare AWV) or G0439 (subsequent Medicare AWV) when the patient has been enrolled in Medicare Part B for 12 months or less. This situation instead calls for billing G0402 (IPPE).
2. Billing for a Medicare AWV when the patient only has Medicare Part A. They must have Part B coverage as well.
3. Using the wrong primary diagnosis code. If the primary diagnosis code is problem-oriented (e.g., diabetes or hypertension), Medicare will most likely deny a claim for an AWV, because AWVs are “well visits.” Instead, list a well code (e.g., Z00.0X, “encounter for general adult exam”) as the primary diagnosis.
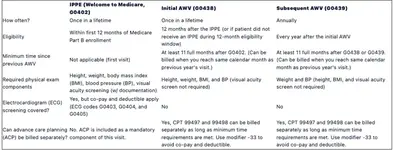
The IPPE also has a slightly different set of required components (e.g., advance care planning and visual acuity screening with documentation of results in the note) than the two types of AWVs (e.g., instrumental activity of daily living and assessment of cognitive function).
What is the difference between a Medicare AWV and a preventive visit
Medicare AWVs consist of three specific visit types statutorily covered by Medicare with no co-pay or deductible. They are the IPPE (the “Welcome to Medicare” visit, G0402), the initial AWV (G0438), and the subsequent AWV (G0439). These visits do not require a comprehensive physical exam. Preventive visits (9938X and 9939X) are covered by commercial/managed care and Medicaid plans and require a comprehensive physical exam. They are also include no co-pay or deductible.
Can a Medicare patient receive a preventive visit
Yes, but traditional Medicare does not cover these visits (9938X and 9939X are statutorily prohibited), so patients with that coverage will have to pay 100% out-of-pocket. However, some Medicare Advantage plans cover both Medicare AWVs (G codes) and non-Medicare (commercial) preventive visits (9938X and 9939X). Medicare Advantage patients would need to check their plan benefits to find out if they have coverage for both.
Is the IPPE the same as the initial AWV
No, the IPPE is the Initial Preventive Physical Examination, also known as the "Welcome to Medicare" visit (G0402), while the initial AWV (G0438) is the patient’s first Medicare AWV following the IPPE. These are two different types of visits, and billing a G0438 when the patient was actually only eligible for a G0402 is a common cause of denials
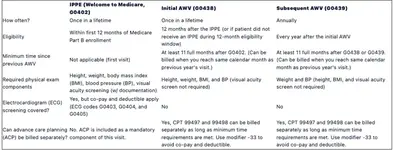
Identifying whether to code for an Initial Preventive Physical Exam (aka the “Welcome to Medicare” visit), an Initial Medicare Annual Wellness Visit (AWV) or a Subsequent Medicare AWV can be tricky.

www.aafp.org