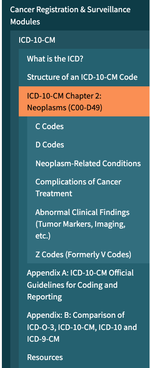
. Chapter 2: Neoplasms (C00-D49)
General Guidelines
Chapter 2 of the ICD-10-CM contains the codes for most benign and all malignant
neoplasms. Certain benign neoplasms, such as prostatic adenomas, may be found in the
specific body system chapters. To properly code a neoplasm, it is necessary to
determine from the record if the neoplasm is benign, in-situ, malignant, or of uncertain
histologic behavior. If malignant, any secondary (metastatic) sites should also be
determined.
Primary malignant neoplasms overlapping site boundaries
A primary malignant neoplasm that overlaps two or more contiguous (next to each
other) sites should be classified to the subcategory/code .8 ('overlapping lesion'),
unless the combination is specifically indexed elsewhere. For multiple neoplasms of
the same site that are not contiguous such as tumors in different quadrants of the
same breast, codes for each site should be assigned.
Malignant neoplasm of ectopic tissue
Malignant neoplasms of ectopic tissue are to be coded to the site of origin
mentioned, e.g., ectopic pancreatic malignant neoplasms involving the stomach are
coded to malignant neoplasm of pancreas, unspecified (C25.9).
The neoplasm table in the Alphabetic Index should be referenced first. However, if the
histological term is documented, that term should be referenced first, rather than going
ICD-10-CM Official Guidelines for Coding andReporting
FY 2022
Page 32 of 115
immediately to the Neoplasm Table, in order to determine which column in the
Neoplasm Table is appropriate. For example, if the documentation indicates “adenoma,”
refer to the term in the Alphabetic Index to review the entries under this term and the
instructional note to “see also neoplasm, by site, benign.” The table provides the proper
code based on the type of neoplasm and the site. It is important to select the proper
column in the table that corresponds to the type of neoplasm. The Tabular List should
then be referenced to verify that the correct code has been selected from the table and
that a more specific site code does not exist.
See Section I.C.21. Factors influencing health status and contact with health services,
Status, for information regarding Z15.0, codes for genetic susceptibility to cancer.
a. Treatment directed at the malignancy
If the treatment is directed at the malignancy, designate the malignancy as the
principal diagnosis.
The only exception to this guideline is if a patient admission/encounter is solely
for the administration of chemotherapy, immunotherapy or external beam
radiation therapy, assign the appropriate Z51.-- code as the first-listed or
principal diagnosis, and the diagnosis or problem for which the service is being
performed as a secondary diagnosis.
b. Treatment of secondary site
When a patient is admitted because of a primary neoplasm with metastasis and
treatment is directed toward the secondary site only, the secondary neoplasm is
designated as the principal diagnosis even though the primary malignancy is still
present.
c. Coding and sequencing of complications
Coding and sequencing of complications associated with the malignancies or
with the therapy thereof are subject to the following guidelines:
1) Anemia associated with malignancy
When admission/encounter is for management of an anemia associated
with the malignancy, and the treatment is only for anemia, the
appropriate code for the malignancy is sequenced as the principal or
first-listed diagnosis followed by the appropriate code for the anemia
(such as code D63.0, Anemia in neoplastic disease).
2) Anemia associated with chemotherapy, immunotherapy and
radiation therapy
When the admission/encounter is for management of an anemia
associated with an adverse effect of the administration of chemotherapy
or immunotherapy and the only treatment is for the anemia, the anemia
code is sequenced first followed by the appropriate codes for the
neoplasm and the adverse effect (T45.1X5-, Adverse effect of
antineoplastic and immunosuppressive drugs).
When the admission/encounter is for management of an anemia
associated with an adverse effect of radiotherapy, the anemia code
should be sequenced first, followed by the appropriate neoplasm code
and code Y84.2, Radiological procedure and radiotherapy as the cause of
abnormal reaction of the patient, or of later complication, without
mention of misadventure at the time of the procedure.
3) Management of dehydration due to the malignancy
When the admission/encounter is for management of dehydration due to
the malignancy and only the dehydration is being treated (intravenous
rehydration), the dehydration is sequenced first, followed by the code(s)
for the malignancy.
4) Treatment of a complication resulting from a surgical
procedure
When the admission/encounter is for treatment of a complication
resulting from a surgical procedure, designate the complication as the
principal or first-listed diagnosis if treatment is directed at resolving the
complication.
d. Primary malignancy previously excised
When a primary malignancy has been previously excised or eradicated from its
site and there is no further treatment directed to that site and there is no evidence
of any existing primary malignancy at that site, a code from category Z85,
Personal history of malignant neoplasm, should be used to indicate the former
site of the malignancy. Any mention of extension, invasion, or metastasis to
another site is coded as a secondary malignant neoplasm to that site. The
secondary site may be the principal or first-listed diagnosis with the Z85 code
used as a secondary code.
e. Admissions/Encounters involving chemotherapy, immunotherapy
and radiation therapy
1) Episode of care involves surgical removal of neoplasm
When an episode of care involves the surgical removal of a neoplasm,
primary or secondary site, followed by adjunct chemotherapy or
radiation treatment during the same episode of care, the code for the
neoplasm should be assigned as principal or first-listed diagnosis.
2) Patient admission/encounter solely for administration of
chemotherapy, immunotherapy and radiation therapy
If a patient admission/encounter is solely for the administration of
chemotherapy, immunotherapy or external beam radiation therapy assign
code Z51.0, Encounter for antineoplastic radiation therapy, or Z51.11,
Encounter for antineoplastic chemotherapy, or Z51.12, Encounter for
antineoplastic immunotherapy as the first-listed or principal diagnosis. If
a patient receives more than one of these therapies during the same
ICD-10-CM Official Guidelines for Coding andReporting
FY 2022
Page 34 of 115
admission more than one of these codes may be assigned, in any
sequence.
The malignancy for which the therapy is being administered should be
assigned as a secondary diagnosis.
If a patient admission/encounter is for the insertion or implantation of
radioactive elements (e.g., brachytherapy) the appropriate code for the
malignancy is sequenced as the principal or first-listed diagnosis. Code
Z51.0 should not be assigned.
3) Patient admitted for radiation therapy, chemotherapy or
immunotherapy and develops complications
When a patient is admitted for the purpose of external beam
radiotherapy, immunotherapy or chemotherapy and develops
complications such as uncontrolled nausea and vomiting or dehydration,
the principal or first-listed diagnosis is Z51.0, Encounter for
antineoplastic radiation therapy, or Z51.11, Encounter for antineoplastic
chemotherapy, or Z51.12, Encounter for antineoplastic immunotherapy
followed by any codes for the complications.
When a patient is admitted for the purpose of insertion or implantation of
radioactive elements (e.g., brachytherapy) and develops complications
such as uncontrolled nausea and vomiting or dehydration, the principal
or first-listed diagnosis is the appropriate code for the malignancy
followed by any codes for the complications.
f. Admission/encounter to determine extent of malignancy
When the reason for admission/encounter is to determine the extent of the
malignancy, or for a procedure such as paracentesis or thoracentesis, the primary
malignancy or appropriate metastatic site is designated as the principal or
first-listed diagnosis, even though chemotherapy or radiotherapy is
administered.
g. Symptoms, signs, and abnormal findings listed in Chapter 18
associated with neoplasms
Symptoms, signs, and ill-defined conditions listed in Chapter 18 characteristic
of, or associated with, an existing primary or secondary site malignancy cannot
be used to replace the malignancy as principal or first-listed diagnosis,
regardless of the number of admissions or encounters for treatment and care of
the neoplasm.
See section I.C.21. Factors influencing health status and contact with health
services, Encounter for prophylactic organ removal.
h. Admission/encounter for pain control/management
See Section I.C.6. for information on coding admission/encounter for pain
control/management.
i. Malignancy in two or more noncontiguous sites
A patient may have more than one malignant tumor in the same organ. These
tumors may represent different primaries or metastatic disease, depending on the
site. Should the documentation be unclear, the provider should be queried as to
the status of each tumor so that the correct codes can be assigned.
j. Disseminated malignant neoplasm, unspecified
Code C80.0, Disseminated malignant neoplasm, unspecified, is for use only in
those cases where the patient has advanced metastatic disease and no known
primary or secondary sites are specified. It should not be used in place of
assigning codes for the primary site and all known secondary sites.
k. Malignant neoplasm without specification of site
Code C80.1, Malignant (primary) neoplasm, unspecified, equates to Cancer,
unspecified. This code should only be used when no determination can be made
as to the primary site of a malignancy. This code should rarely be used in the
inpatient setting.
l. Sequencing of neoplasm codes
1) Encounter for treatment of primary malignancy
If the reason for the encounter is for treatment of a primary malignancy,
assign the malignancy as the principal/first-listed diagnosis. The primary
site is to be sequenced first, followed by any metastatic sites.
2) Encounter for treatment of secondary malignancy
When an encounter is for a primary malignancy with metastasis and
treatment is directed toward the metastatic (secondary) site(s) only, the
metastatic site(s) is designated as the principal/first-listed diagnosis. The
primary malignancy is coded as an additional code.
3) Malignant neoplasm in a pregnant patient
When a pregnant patient has a malignant neoplasm, a code from
subcategory O9A.1-, Malignant neoplasm complicating pregnancy,
childbirth, and the puerperium, should be sequenced first, followed by
the appropriate code from Chapter 2 to indicate the type of neoplasm.
4) Encounter for complication associated with a neoplasm
When an encounter is for management of a complication associated with
a neoplasm, such as dehydration, and the treatment is only for the
complication, the complication is coded first, followed by the appropriate
code(s) for the neoplasm.
The exception to this guideline is anemia. When the admission/encounter
is for management of an anemia associated with the malignancy, and the
treatment is only for anemia, the appropriate code for the malignancy is
sequenced as the principal or first-listed diagnosis followed by code
D63.0, Anemia in neoplastic disease.
5) Complication from surgical procedure for treatment of a
neoplasm
When an encounter is for treatment of a complication resulting from a
surgical procedure performed for the treatment of the neoplasm,
designate the complication as the principal/first-listed diagnosis. See the
guideline regarding the coding of a current malignancy versus personal
history to determine if the code for the neoplasm should also be assigned.
6) Pathologic fracture due to a neoplasm
When an encounter is for a pathological fracture due to a neoplasm, and
the focus of treatment is the fracture, a code from subcategory M84.5,
Pathological fracture in neoplastic disease, should be sequenced first,
followed by the code for the neoplasm.
If the focus of treatment is the neoplasm with an associated pathological
fracture, the neoplasm code should be sequenced first, followed by a
code from M84.5 for the pathological fracture.
m. Current malignancy versus personal history of malignancy
When a primary malignancy has been excised but further treatment, such as an
additional surgery for the malignancy, radiation therapy or chemotherapy is
directed to that site, the primary malignancy code should be used until treatment
is completed.
When a primary malignancy has been previously excised or eradicated from its
site, there is no further treatment (of the malignancy) directed to that site, and
there is no evidence of any existing primary malignancy at that site, a code from
category Z85, Personal history of malignant neoplasm, should be used to
indicate the former site of the malignancy.
Codes from subcategories Z85.0 – Z85.85 should only be assigned for the
former site of a primary malignancy, not the site of a secondary malignancy.
Code Z85.89 may be assigned for the former site(s) of either a primary or
secondary malignancy.
See Section I.C.21. Factors influencing health status and contact with health
services, History (of)
n. Leukemia, Multiple Myeloma, and Malignant Plasma Cell
Neoplasms in remission versus personal history
The categories for leukemia, and category C90, Multiple myeloma and
malignant plasma cell neoplasms, have codes indicating whether or not the
leukemia has achieved remission. There are also codes Z85.6, Personal history
of leukemia, and Z85.79, Personal history of other malignant neoplasms of
lymphoid, hematopoietic and related tissues. If the documentation is unclear as
to whether the leukemia has achieved remission, the provider should be queried.
See Section I.C.21. Factors influencing health status and contact with health
services, History (of)
o. Aftercare following surgery for neoplasm
See Section I.C.21. Factors influencing health status and contact with health
services, Aftercare
p. Follow-up care for completed treatment of a malignancy
See Section I.C.21. Factors influencing health status and contact with health
services, Follow-up
q. Prophylactic organ removal for prevention of malignancy
See Section I.C. 21, Factors influencing health status and contact with health
services, Prophylactic organ removal
r. Malignant neoplasm associated with transplanted organ
A malignant neoplasm of a transplanted organ should be coded as a transplant
complication. Assign first the appropriate code from category T86.-,
Complications of transplanted organs and tissue, followed by code C80.2,
Malignant neoplasm associated with transplanted organ. Use an additional code
for the specific malignancy.
s. Breast Implant Associated Anaplastic Large Cell Lymphoma
Breast implant associated anaplastic large cell lymphoma (BIA-ALCL) is a
type of lymphoma that can develop around breast implants. Assign code
C84.7A, Anaplastic large cell lymphoma, ALK-negative, breast, for BIAALCL. Do not assign a complication code from chapter 19.
General Guidelines
Chapter 2 of the ICD-10-CM contains the codes for most benign and all malignant
neoplasms. Certain benign neoplasms, such as prostatic adenomas, may be found in the
specific body system chapters. To properly code a neoplasm, it is necessary to
determine from the record if the neoplasm is benign, in-situ, malignant, or of uncertain
histologic behavior. If malignant, any secondary (metastatic) sites should also be
determined.
Primary malignant neoplasms overlapping site boundaries
A primary malignant neoplasm that overlaps two or more contiguous (next to each
other) sites should be classified to the subcategory/code .8 ('overlapping lesion'),
unless the combination is specifically indexed elsewhere. For multiple neoplasms of
the same site that are not contiguous such as tumors in different quadrants of the
same breast, codes for each site should be assigned.
Malignant neoplasm of ectopic tissue
Malignant neoplasms of ectopic tissue are to be coded to the site of origin
mentioned, e.g., ectopic pancreatic malignant neoplasms involving the stomach are
coded to malignant neoplasm of pancreas, unspecified (C25.9).
The neoplasm table in the Alphabetic Index should be referenced first. However, if the
histological term is documented, that term should be referenced first, rather than going
ICD-10-CM Official Guidelines for Coding andReporting
FY 2022
Page 32 of 115
immediately to the Neoplasm Table, in order to determine which column in the
Neoplasm Table is appropriate. For example, if the documentation indicates “adenoma,”
refer to the term in the Alphabetic Index to review the entries under this term and the
instructional note to “see also neoplasm, by site, benign.” The table provides the proper
code based on the type of neoplasm and the site. It is important to select the proper
column in the table that corresponds to the type of neoplasm. The Tabular List should
then be referenced to verify that the correct code has been selected from the table and
that a more specific site code does not exist.
See Section I.C.21. Factors influencing health status and contact with health services,
Status, for information regarding Z15.0, codes for genetic susceptibility to cancer.
a. Treatment directed at the malignancy
If the treatment is directed at the malignancy, designate the malignancy as the
principal diagnosis.
The only exception to this guideline is if a patient admission/encounter is solely
for the administration of chemotherapy, immunotherapy or external beam
radiation therapy, assign the appropriate Z51.-- code as the first-listed or
principal diagnosis, and the diagnosis or problem for which the service is being
performed as a secondary diagnosis.
b. Treatment of secondary site
When a patient is admitted because of a primary neoplasm with metastasis and
treatment is directed toward the secondary site only, the secondary neoplasm is
designated as the principal diagnosis even though the primary malignancy is still
present.
c. Coding and sequencing of complications
Coding and sequencing of complications associated with the malignancies or
with the therapy thereof are subject to the following guidelines:
1) Anemia associated with malignancy
When admission/encounter is for management of an anemia associated
with the malignancy, and the treatment is only for anemia, the
appropriate code for the malignancy is sequenced as the principal or
first-listed diagnosis followed by the appropriate code for the anemia
(such as code D63.0, Anemia in neoplastic disease).
2) Anemia associated with chemotherapy, immunotherapy and
radiation therapy
When the admission/encounter is for management of an anemia
associated with an adverse effect of the administration of chemotherapy
or immunotherapy and the only treatment is for the anemia, the anemia
code is sequenced first followed by the appropriate codes for the
neoplasm and the adverse effect (T45.1X5-, Adverse effect of
antineoplastic and immunosuppressive drugs).
When the admission/encounter is for management of an anemia
associated with an adverse effect of radiotherapy, the anemia code
should be sequenced first, followed by the appropriate neoplasm code
and code Y84.2, Radiological procedure and radiotherapy as the cause of
abnormal reaction of the patient, or of later complication, without
mention of misadventure at the time of the procedure.
3) Management of dehydration due to the malignancy
When the admission/encounter is for management of dehydration due to
the malignancy and only the dehydration is being treated (intravenous
rehydration), the dehydration is sequenced first, followed by the code(s)
for the malignancy.
4) Treatment of a complication resulting from a surgical
procedure
When the admission/encounter is for treatment of a complication
resulting from a surgical procedure, designate the complication as the
principal or first-listed diagnosis if treatment is directed at resolving the
complication.
d. Primary malignancy previously excised
When a primary malignancy has been previously excised or eradicated from its
site and there is no further treatment directed to that site and there is no evidence
of any existing primary malignancy at that site, a code from category Z85,
Personal history of malignant neoplasm, should be used to indicate the former
site of the malignancy. Any mention of extension, invasion, or metastasis to
another site is coded as a secondary malignant neoplasm to that site. The
secondary site may be the principal or first-listed diagnosis with the Z85 code
used as a secondary code.
e. Admissions/Encounters involving chemotherapy, immunotherapy
and radiation therapy
1) Episode of care involves surgical removal of neoplasm
When an episode of care involves the surgical removal of a neoplasm,
primary or secondary site, followed by adjunct chemotherapy or
radiation treatment during the same episode of care, the code for the
neoplasm should be assigned as principal or first-listed diagnosis.
2) Patient admission/encounter solely for administration of
chemotherapy, immunotherapy and radiation therapy
If a patient admission/encounter is solely for the administration of
chemotherapy, immunotherapy or external beam radiation therapy assign
code Z51.0, Encounter for antineoplastic radiation therapy, or Z51.11,
Encounter for antineoplastic chemotherapy, or Z51.12, Encounter for
antineoplastic immunotherapy as the first-listed or principal diagnosis. If
a patient receives more than one of these therapies during the same
ICD-10-CM Official Guidelines for Coding andReporting
FY 2022
Page 34 of 115
admission more than one of these codes may be assigned, in any
sequence.
The malignancy for which the therapy is being administered should be
assigned as a secondary diagnosis.
If a patient admission/encounter is for the insertion or implantation of
radioactive elements (e.g., brachytherapy) the appropriate code for the
malignancy is sequenced as the principal or first-listed diagnosis. Code
Z51.0 should not be assigned.
3) Patient admitted for radiation therapy, chemotherapy or
immunotherapy and develops complications
When a patient is admitted for the purpose of external beam
radiotherapy, immunotherapy or chemotherapy and develops
complications such as uncontrolled nausea and vomiting or dehydration,
the principal or first-listed diagnosis is Z51.0, Encounter for
antineoplastic radiation therapy, or Z51.11, Encounter for antineoplastic
chemotherapy, or Z51.12, Encounter for antineoplastic immunotherapy
followed by any codes for the complications.
When a patient is admitted for the purpose of insertion or implantation of
radioactive elements (e.g., brachytherapy) and develops complications
such as uncontrolled nausea and vomiting or dehydration, the principal
or first-listed diagnosis is the appropriate code for the malignancy
followed by any codes for the complications.
f. Admission/encounter to determine extent of malignancy
When the reason for admission/encounter is to determine the extent of the
malignancy, or for a procedure such as paracentesis or thoracentesis, the primary
malignancy or appropriate metastatic site is designated as the principal or
first-listed diagnosis, even though chemotherapy or radiotherapy is
administered.
g. Symptoms, signs, and abnormal findings listed in Chapter 18
associated with neoplasms
Symptoms, signs, and ill-defined conditions listed in Chapter 18 characteristic
of, or associated with, an existing primary or secondary site malignancy cannot
be used to replace the malignancy as principal or first-listed diagnosis,
regardless of the number of admissions or encounters for treatment and care of
the neoplasm.
See section I.C.21. Factors influencing health status and contact with health
services, Encounter for prophylactic organ removal.
h. Admission/encounter for pain control/management
See Section I.C.6. for information on coding admission/encounter for pain
control/management.
i. Malignancy in two or more noncontiguous sites
A patient may have more than one malignant tumor in the same organ. These
tumors may represent different primaries or metastatic disease, depending on the
site. Should the documentation be unclear, the provider should be queried as to
the status of each tumor so that the correct codes can be assigned.
j. Disseminated malignant neoplasm, unspecified
Code C80.0, Disseminated malignant neoplasm, unspecified, is for use only in
those cases where the patient has advanced metastatic disease and no known
primary or secondary sites are specified. It should not be used in place of
assigning codes for the primary site and all known secondary sites.
k. Malignant neoplasm without specification of site
Code C80.1, Malignant (primary) neoplasm, unspecified, equates to Cancer,
unspecified. This code should only be used when no determination can be made
as to the primary site of a malignancy. This code should rarely be used in the
inpatient setting.
l. Sequencing of neoplasm codes
1) Encounter for treatment of primary malignancy
If the reason for the encounter is for treatment of a primary malignancy,
assign the malignancy as the principal/first-listed diagnosis. The primary
site is to be sequenced first, followed by any metastatic sites.
2) Encounter for treatment of secondary malignancy
When an encounter is for a primary malignancy with metastasis and
treatment is directed toward the metastatic (secondary) site(s) only, the
metastatic site(s) is designated as the principal/first-listed diagnosis. The
primary malignancy is coded as an additional code.
3) Malignant neoplasm in a pregnant patient
When a pregnant patient has a malignant neoplasm, a code from
subcategory O9A.1-, Malignant neoplasm complicating pregnancy,
childbirth, and the puerperium, should be sequenced first, followed by
the appropriate code from Chapter 2 to indicate the type of neoplasm.
4) Encounter for complication associated with a neoplasm
When an encounter is for management of a complication associated with
a neoplasm, such as dehydration, and the treatment is only for the
complication, the complication is coded first, followed by the appropriate
code(s) for the neoplasm.
The exception to this guideline is anemia. When the admission/encounter
is for management of an anemia associated with the malignancy, and the
treatment is only for anemia, the appropriate code for the malignancy is
sequenced as the principal or first-listed diagnosis followed by code
D63.0, Anemia in neoplastic disease.
5) Complication from surgical procedure for treatment of a
neoplasm
When an encounter is for treatment of a complication resulting from a
surgical procedure performed for the treatment of the neoplasm,
designate the complication as the principal/first-listed diagnosis. See the
guideline regarding the coding of a current malignancy versus personal
history to determine if the code for the neoplasm should also be assigned.
6) Pathologic fracture due to a neoplasm
When an encounter is for a pathological fracture due to a neoplasm, and
the focus of treatment is the fracture, a code from subcategory M84.5,
Pathological fracture in neoplastic disease, should be sequenced first,
followed by the code for the neoplasm.
If the focus of treatment is the neoplasm with an associated pathological
fracture, the neoplasm code should be sequenced first, followed by a
code from M84.5 for the pathological fracture.
m. Current malignancy versus personal history of malignancy
When a primary malignancy has been excised but further treatment, such as an
additional surgery for the malignancy, radiation therapy or chemotherapy is
directed to that site, the primary malignancy code should be used until treatment
is completed.
When a primary malignancy has been previously excised or eradicated from its
site, there is no further treatment (of the malignancy) directed to that site, and
there is no evidence of any existing primary malignancy at that site, a code from
category Z85, Personal history of malignant neoplasm, should be used to
indicate the former site of the malignancy.
Codes from subcategories Z85.0 – Z85.85 should only be assigned for the
former site of a primary malignancy, not the site of a secondary malignancy.
Code Z85.89 may be assigned for the former site(s) of either a primary or
secondary malignancy.
See Section I.C.21. Factors influencing health status and contact with health
services, History (of)
n. Leukemia, Multiple Myeloma, and Malignant Plasma Cell
Neoplasms in remission versus personal history
The categories for leukemia, and category C90, Multiple myeloma and
malignant plasma cell neoplasms, have codes indicating whether or not the
leukemia has achieved remission. There are also codes Z85.6, Personal history
of leukemia, and Z85.79, Personal history of other malignant neoplasms of
lymphoid, hematopoietic and related tissues. If the documentation is unclear as
to whether the leukemia has achieved remission, the provider should be queried.
See Section I.C.21. Factors influencing health status and contact with health
services, History (of)
o. Aftercare following surgery for neoplasm
See Section I.C.21. Factors influencing health status and contact with health
services, Aftercare
p. Follow-up care for completed treatment of a malignancy
See Section I.C.21. Factors influencing health status and contact with health
services, Follow-up
q. Prophylactic organ removal for prevention of malignancy
See Section I.C. 21, Factors influencing health status and contact with health
services, Prophylactic organ removal
r. Malignant neoplasm associated with transplanted organ
A malignant neoplasm of a transplanted organ should be coded as a transplant
complication. Assign first the appropriate code from category T86.-,
Complications of transplanted organs and tissue, followed by code C80.2,
Malignant neoplasm associated with transplanted organ. Use an additional code
for the specific malignancy.
s. Breast Implant Associated Anaplastic Large Cell Lymphoma
Breast implant associated anaplastic large cell lymphoma (BIA-ALCL) is a
type of lymphoma that can develop around breast implants. Assign code
C84.7A, Anaplastic large cell lymphoma, ALK-negative, breast, for BIAALCL. Do not assign a complication code from chapter 19.