Billing For Telehealth Encounters
An introductory guide on fee for service
Some great tips in here!
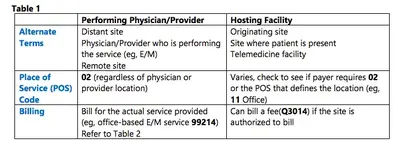
Originating Site
Distant Site
Eligible Providers
Codes
Modifiers
Place of Service Codes
The Rest of the POS Codes
Revenue Codes
Services 'Evaluation and Management CPT Codes
Other E/M Services
Communication Technology Based Services (CTBS) – Non-Telehealth Technology Services
Remote Evaluation and Virtual Check-in
Care Management (CM) Codes
Remote Physiological or Patient Monitoring (RPM)18 Remote Therapeutic Monitoring (RTM)
eConsult or Interprofessional Consultation Codes & eVisit ...
The Center for Connected Health Policy (CCHP) is providing this informational billing guide to assist those who have questions regarding telehealth billing in general and specifically, post-PHE. The guide is primarily about Medicare fee-for-service billing as policies vary from state-to-state for Medicaid and commercial payers. It is not meant to be a guarantee of reimbursement for services rendered via telehealth, but to act as a guide to clarify certain policies related to: • telehealth billing and reimbursement • requirements applicable during 2023 (in the post-PHE environment)
• permanent telehealth billing requirements past the temporary grace period post-PHE The guide will outline the policies in place for 2023, as well as permanent Medicare policy as we currently know it. Keep in mind, policy can change rapidly and frequently. ) PE
Permanent Medicare Policy
Outpatient Prospective Payment System (OPPS)
Three codes were added to the CMS Telehealth List on May 9, 2023 and are discussed below.
Since the PHE allowed Partial Hospitalization and Intensive Outpatient Program services to take place in a patient’s home via telehealth, the following occurred:
In the CY 2023 Outpatient Prospective Payment System final rule, CMS established a policy that allows clinical staff of hospitals to provide certain mental health services via a telecommunications system to patients in their homes after the PHE. They established 3 new codes and code descriptors (C7900-C7902) for these remote mental health services furnished by hospital outpatient department (HOPD) staff. Because HCPCS codes C7900 – C7902 describe remote mental health services furnished by hospital staff to a patient in their home, and the statute prohibits Partial Hospitalization Program (PHP) services from being furnished in an individual’s home, these are not considered PHP services, and CMHCs can’t furnish these remote services. However, patients receiving PHP services from a CMHC or hospital-based PHP could receive the remote mental health services from clinical staff of a HOPD. The policy discussion starts at 87 FR 72014.
The code definitions are as follows:
• C7900 - Service for diagnosis, evaluation, or treatment of a mental health or substance use disorder, initial 15-29 minutes, provided remotely by hospital staff who are licensed to provide mental health services under applicable state law(s), when the patient is in their home, and there is no associated professional service
• C7901 - Service for diagnosis, evaluation, or treatment of a mental health or substance use disorder, initial 30-60 minutes, provided remotely by hospital staff who are licensed to provided mental health services under applicable state law(s), when the patient is in their home, and there is no associated professional service
• C7902 - Service for diagnosis, evaluation, or treatment of a mental health or substance use disorder, each additional 15 minutes, provided remotely by hospital staff who are licensed to provide mental health services under applicable state law(s), when the patient is in their home, and there is no associated professional service (list separately in addition to code for primary service)


acrobat.adobe.com